
Feb 23, 2021
Looking back to look forward

Nurses, nurse leaders, nurse champions and allies from across the country will virtually gather Wednesday to reflect on the profession’s achievements since the release of the 2010 Institute of Medicine report The Future of Nursing: Leading Change, Advancing Health.
More than a decade ago, that report called for nurses to seize the opportunities created by the Affordable Care Act’s expansion of access to care. It described several new capacities the profession would need to realize to achieve the goal of quality health care for all in America.
In 2021, many of those new capacities have been fully activated, while others are well on their way to becoming real. The profession can take pride in being more educated and more influential than ever before. The Future of Nursing: Campaign for Action’s dashboard indicators demonstrate this steady progress.
Yet nurses are also well aware that the dream of quality health care for all has not been realized. They are deeply concerned about new challenges like COVID-19 and old enemies like racism and misogyny. They do not want to merely congratulate themselves on their achievements, but figure out new ways to put them to work for those they serve.
A new Future of Nursing report, expected to be released this spring, will further explore these challenges. But in the meantime, Campaign experts are reflecting on the achievements described in the dashboard and what they mean to nurses now.
The Campaign is a national initiative of AARP Foundation, AARP and the Robert Wood Johnson Foundation created in 2010 to implement recommendations from the first Future of Nursing report. The Center to Champion Nursing in America, an initiative of those same organizations, runs the Campaign, which is directed by Susan B. Hassmiller, PhD, RN, FAAN, senior adviser for nursing, Robert Wood Johnson Foundation and senior scholar in residence and senior advisor on nursing to the present of the National Academy of Medicine, and Susan C. Reinhard, senior vice president and director, AARP Public Policy Institute and chief strategist for the Center to Champion Nursing in America and Family Caregiving Initiatives.
Diversity in Nursing and Health Equity
Ten years ago, more than 80 percent of the RN workforce was white, and men made up just seven percent of the RN population. The 2010 Future of Nursing report noted these demographic gaps between the nursing profession and the patients it serves. In the years since, diversifying the nursing workforce has become an increasingly important issue for the Campaign of Action as well as other health care institutions.

Kupiri Ackerman-Barger, PhD, RN, FAAN, a Campaign advisor on diversity and inclusion
The dashboard’s latest diversity numbers point to incremental progress on this front, as they have for many years. Kupiri Ackerman-Barger, PhD, RN, FAAN, is associate dean of Health Equity, Diversity and Inclusion, as well as an associate clinical professor at the University of California Davis Betty Irene Moore School of Nursing, and a Campaign advisor on diversity and inclusion. She says it is essential that the nursing profession understands this information in context. Plenty of work still has to be done to achieve a diverse nursing workforce, much less empower that workforce to realize health equity, she said.
 “We see these tiny increases in diversity each year,” Ackerman-Barger said. “We are not at a standstill, we are not going backwards, but we need to understand that this is a complex, structural problem that won’t be fixed with incremental change,” she said. “At the rate we are going, it is going to be another fifty years or so before we meet the benchmark of the nursing profession matching the American population — that’s too slow.”
“We see these tiny increases in diversity each year,” Ackerman-Barger said. “We are not at a standstill, we are not going backwards, but we need to understand that this is a complex, structural problem that won’t be fixed with incremental change,” she said. “At the rate we are going, it is going to be another fifty years or so before we meet the benchmark of the nursing profession matching the American population — that’s too slow.”
Ackerman-Barger takes hope from the fact that more and more people are understanding the importance of a diverse healthcare workforce — a development she says the Campaign helped bring about.
But now a new conversation needs to begin, she said. The coming decade will require greater critical thinking about the best actions to take to achieve workforce diversity. Issues of race and gender will also need to be understood with greater nuance in order to serve a more diverse population.
“Patients tend to have more satisfaction when they can receive care from someone with a background similar to themselves,” she said. “It’s also an issue of trust. Many communities don’t trust the health care system — for good reasons, historical and current. When we have representation from those communities, that engenders understanding and trust. When patients trust us, they are more likely to communicate with providers or be part of a plan for disease prevention.”
This will require innovation in data collection and program development. For example, Ackerman-Barger points out that while the nursing workforce is becoming more diverse as a whole, there is also stratification in the opportunities available for different groups. While the Campaign has successfully pushed for more baccalaureate-trained nurses, these graduates tend to be more white than the nursing population as a whole. Meanwhile, licensed vocational nurses (LVN) are disproportionately people of color.
“We have to better understand that pipeline,” she said. “It’s a matter of equity, because the LVN positions do not pay as much, they often work long hours in long-term care facilities, and they have a much harder path for career growth. I love our dashboard, but that complexity is currently missing.”
Along with colleagues from the Campaign, Ackerman-Barger recently hosted a Health Equity Action Forum that explored the opportunities and challenges for new nurses from historically underrepresented groups. She explained that looking at the issue of men in nursing can help illuminate the complex interplay of race, gender, and other factors that the profession will need to understand moving forward.
 Men are still an underrepresented population in nursing. According to the dashboard, graduates of pre-licensure RN programs are 13.9 percent male, while the population of the United States is 49.2 percent male.
Men are still an underrepresented population in nursing. According to the dashboard, graduates of pre-licensure RN programs are 13.9 percent male, while the population of the United States is 49.2 percent male.
Yet Ackerman-Barger points out that just because men are underrepresented, this does not mean that they are underserved. In fact, there appears to be an opportunity gap in nursing similar to the ones in other fields.
“We need to have conversations about what it means to be a man in nursing and how we need to buck gender stereotypes,” Ackerman-Barger said. “But we also need to acknowledge that men in nursing tend to make more money and get hired into prestigious positions at a higher rate than women do.”
Among other subjects, participants in the Health Equity Action Forum considered how to recruit more Black men into nursing — an opportunity to significantly advance health equity, Ackerman-Barger said.
“It’s a really important conversation,” she said. “In nursing, we have a small number of men and a small number of people of color, so the number of Black men is tiny. Yet when it comes to health disparities, there are so many issues that are particular to Black men and where we need to have the perspective of Black men in talking about what is missing from our policies, research, and curricula.”
This conversation gave Ackerman-Barger hope for what the next decade of conversations about diversity in nursing could look like, she said. Plans for the future of the dashboard’s health equity metrics include adding new demographic indicators like LGBTQ status. But just as important will be understanding the greater vision for social justice this data should inform.
“One mistake people can make is thinking that any one of these things is the answer,” she said. “Doing something like recruiting more Black men into nursing won’t make health disparities go away on its own. We need to acknowledge that we are addressing racial differences in health outcomes that in some cases start as early as pre-school. So all of these efforts are just strands in the effort to fix a complicated system.”
Education and Leadership
Perhaps the most widely recognized outcome of the 2010 report was the shift to bachelor’s level education in nursing. Less than half of the RN workforce in 2010 held a bachelor’s degree. Today, it has increased to more than 59 percent. Patricia Polansky, RN, MS, director of program development and implementation for the Center to Champion Nursing in America, says that increase has led to a critical “tipping point.”

Patricia Polansky, RN, MS, director of program development and implementation for the Center to Champion Nursing in America
“Academic progression has become a formal movement in the profession,” Polansky said. “That did not exist prior to the 2010 report. All aspects of nursing became involved, and we’ve really seen lots of truly innovative ways to transform nursing education and generate more baccalaureate degree nurses.”
The emphasis on greater education has helped the profession respond to problems no one could imagine in 2010, Polansky argued.
 “The committee rightly saw that the complexity of health care was increasing and we would face enormous challenges going forward, so we would need a more highly educated nursing workforce,” she said. “Obviously COVID-19 and everything else that has happened in the past year has proven that that is true.”
“The committee rightly saw that the complexity of health care was increasing and we would face enormous challenges going forward, so we would need a more highly educated nursing workforce,” she said. “Obviously COVID-19 and everything else that has happened in the past year has proven that that is true.”
 Doctoral education for nurses was also an important goal of the 2010 report. The dashboard shows that the profession has succeeded on this indicator more than anyone could have imagined. The report called for a doubling of doctorally trained nurses by the end of the decade. But because of the explosion in advanced practice doctorate programs, the number has increased by more than 350 percent.
Doctoral education for nurses was also an important goal of the 2010 report. The dashboard shows that the profession has succeeded on this indicator more than anyone could have imagined. The report called for a doubling of doctorally trained nurses by the end of the decade. But because of the explosion in advanced practice doctorate programs, the number has increased by more than 350 percent.
Polansky said doctorally trained nurses have important contributions to make to American health care.
“Every profession needs PhDs, and we should be proud that we achieved that goal,” she said. “But we now also have doctorally prepared people in every clinical setting under the sun. That is going to make us more ambitious about policymaking and leading change. It will have an exponential impact.”
Nurses are also making a new kind of impact through service on institutions’ boards and other leadership groups. This was one of the report’s most innovative recommendations, Polansky said. She called the data on nurses’ board participation before 2010 “abysmal.”
 But this year the dashboard showed that the number of nurses registered as board members and serving on other leadership groups reached more than 10,000 for the first time.
But this year the dashboard showed that the number of nurses registered as board members and serving on other leadership groups reached more than 10,000 for the first time.
“Nurses are naturally born problem-solvers — tenacious, tireless,” Polansky said. “You see that in all kinds of clinical settings. Those are qualities that people need on boards and committees and task forces. If we had more nurses in leadership, we might not have terrible public health situations like we saw with the water in Flint, Michigan.”
The general public may not be as aware of nurses’ educational and leadership achievements as Polansky would like. But she said that in the aggregate, the past decade’s advances will help the profession stay worthy of patients’ trust.
“When patients interact with a nurse, they may not know their education level or professional training,” she said. “But they feel the competence that is required for the situation in which they need care. It all goes back to that idea of nursing as the most trusted profession, which the public has voted us year after year. Everybody knows what a nurse is, who a nurse is — it’s that person who will care for you from before you are born until the day you die.”
Access to Care
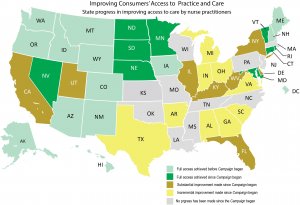
Another significant dashboard indicator focuses on how many people have access to that high-quality nursing care. The Center to Champion Nursing in America, housed at AARP, constantly has its eyes on how many states allow advanced practice registered nurses to practice to the full extent of their education and expertise. In 2020, significant progress was made in new laws passed by California, Florida and Massachusetts.
 The most important change occurred at the federal level. The 2020 CARES Act allowed nurse practitioners, clinical nurse specialists, and physician assistants to certify for Medicare-supported health care. Prior to this law, APRNs’ patients had to wait for a physician to certify that home health care was required.
The most important change occurred at the federal level. The 2020 CARES Act allowed nurse practitioners, clinical nurse specialists, and physician assistants to certify for Medicare-supported health care. Prior to this law, APRNs’ patients had to wait for a physician to certify that home health care was required.

Winifred V. Quinn, PhD, FAANP(H) director of advocacy and consumer affairs at the Center to Champion Nursing in America
These changes will result in material improvements to patients’ lives, said Winifred V. Quinn, PhD, FAANP(H) director of advocacy and consumer affairs at the Center to Champion Nursing in America.
“From the patient experience, a delay of care could lead to unnecessary visits to the emergency room or unnecessary hospitalizations, perhaps worse,” Quinn said. “This is about you being able to get the care when and where you need it. You should be able to see your nurse practitioner and obtain all necessary care without delay during and following that visit.”
For Quinn, these improvements in California, Florida, Massachusetts and at the federal level represent an important achievement that builds upon a decade advocating for reform in access to care policies.
Yet while every change in state and federal laws is important, Quinn argued, just as significant is the narrative the Campaign constructed around these reforms.
“The access to APRN care issue is typically framed as a binary one — nurses versus physicians,” she said. “But we see it as a consumer access to care issue. When patients obtain care when and where they need it, their health is improved and family caregivers’ stress is reduced.”
This reframing helped win the support of a wide variety of stakeholders across the political spectrum, Quinn said.
“Free enterprise organizations, consumer groups, hospitals associations, insurers, and retail clinics have all supported state legislation modernizing APRN laws,” she said.
All of this work resulted in a messaging platform that helped drive advocacy in states where advocates had not previously succeeded.
The work of access to care reform will continue for years to come. Quinn is thrilled by the fact that last year’s reforms brought the total number of states with full access to care to 23. These states include 71.8 million people. The other 27 states and 257 million Americans who do not have direct access to APRN care are never far from her mind.
“Policymakers need to understand that this is an access to care issue, not a power struggle between two clinical sectors, especially when hundreds of thousands of Americans have unnecessarily died this year,” she said.
This type of thinking will also be essential in connecting the Campaign’s legislative agenda to emerging issues of health equity, many of which are expected to be highlighted in the upcoming Future of Nursing report.
“The opposition is making the argument that by modernizing APRN laws, people in underserved communities will receive second-class care,” Quinn said. “That is immoral. With the egregious health disparities that exist in the nation, we must deploy and make available every highly-skilled clinicians to ensure that all people, especially those who experience the worst disparities, receive high quality care when and where they need it.”
Dashboard data analysis by Nicole Rozko, MS, project manager at the Center to Champion Nursing in America.
